Video EEG Test
What Is A Video EEG Test?
A video EEG (electroencephalograph) records what you are doing or experiencing on video while an EEG test records the electrical activity of the brain or brainwaves. The purpose is to be able to see what happens when you have a seizure or an event that is suspected to be a seizure. The video is compared to what the EEG records at the same time. Sounds that occur during the testing are also recorded to pick up if a person talks or makes sounds during an event. By doing this, doctors reading the EEG can tell if the event is related to abnormal electrical activity in the brain. If so, then doctors would call this a seizure related to epilepsy.
Video EEG is helpful to:
- Determine if events with unusual features are actually epileptic seizures.
- Identify the type of seizures (like absence seizures) and their frequency
- Find the region of the brain where seizures begin. Locating the exact region is vital if epilepsy surgery is being considered.
Other names for video EEGs include EEG telemetry, EEG monitoring, or video EEG monitoring.
Where Are Video EEG Tests Done?
Hospital Video EEG
Video EEG tests are usually done in a hospital setting where seizures can be monitored in a safe way. Since seizures are unpredictable, they may not occur during regular EEG monitoring. When a person is in the hospital for video EEG testing, seizure medications can be lowered to help provoke seizures so they can be recorded.
Some people have certain seizure triggers. It is helpful to identify triggers which can help induce a seizure. During video EEG testing, sometimes doctors will provoke seizures using your personal seizure triggers.
The length of testing varies based on how often a person usually has seizures, the type of seizures, and why the monitoring is being done. Testing may take a few days, a week, or more.
At-home or Outpatient Video EEG
Video EEG tests can be done at home or at an outpatient center, like an EEG lab.
In some EEG labs, a person may be monitored by EEG and video over a number of hours in one day. This is good for people with seizure types that occur frequently, happen at specific times of the day, or can be easily and safely triggered (for example by flashing lights).
Some centers can send video equipment home. At-home testing may help record a person's activity and seizures during their daily activities and during sleep. This is hard to do if someone lives alone. Someone else is needed to help with the equipment and help the person during a seizure.
Due to safety risks, seizure medications are generally not lowered for EEG testing done outside of a hospital.
What Happens During Video EEG Tests?
Many people living with epilepsy have likely experienced a standard EEG test. However, video EEG testing is a bit different than a regular EEG. Additional actions are taken to help record seizure activity. This will help your healthcare team to make better decisions about how to treat your seizures.
- The EEG leads are placed on your head with a special paste called collodion. In contrast, most short, outpatient EEGs are done using a cap, or with a different type of paste. The head (and electrodes) are usually covered by a cap or gauze dressing.
- If the test is done in a hospital, you are admitted to a room on the epilepsy monitoring unit (EMU) where the EEG, audio, and video recording can be done.
- The electrodes are connected to a wire or cord that is attached to a cassette. The cord may also be connected to a special EEG connection in the wall or to a nearby machine. Increasingly, wireless systems are being used in monitoring rooms.
- During the monitoring, the doctors may lower your medications so that seizures are more likely to occur. Sometimes other things are done to trigger seizures, such as sleep deprivation, flashing lights or exercise.
Sometimes lowering medications may lead to more seizures than usual. Worse seizures are possible or one that is longer than usual. If your medicine is reduced you may need an IV placed to a longer seizure. Doctors and nurses may need to give you seizure medications that act quickly to stop long or repeated seizures if they occur during the testing.
What Is Done To Keep Me (Or My Loved One) Safe?
Many safety steps will be taken when testing is done in the hospital. Epilepsy monitoring units have different physical layouts that allow staff to watch you closely. Below are some examples of safety strategies that may be used:
- You may not be allowed to get up and walk around on your own. What you can do will depend on a few factors such as your seizure type, how often they occur, and the environment. When out of bed, you may need a staff member with you. They may place a belt around your waist or place you in a ceiling sling to keep you from falling if a seizure occurs while walking.
- You will be asked to sit on top of the bed, within camera view so good video recordings can be obtained.
- Sometimes during or after seizures, a person may try to get out of bed, run or pull at electrodes. This usually happens when a person is confused or not aware of what is going on. If you try to get out of bed, the staff will stand next to you and walk with you in the room making sure that you do not fall. In some cases, you may be asked to wear mitts on your hands to protect you from pulling out electrodes.
- Pads are put on the side rails of the bed to keep you from hurting yourself (in case arms or legs hit the side rails during a seizure).
- Oxygen, suction machine, and other safety equipment is kept nearby, just in case they are needed during a long seizure.
- An intravenous line is often placed if medicine is reduced or stopped in case you have a longer seizure which requires medicine to stop it.
Helpful Tips
Preparing for a video EEG has many similarities to preparing for a regular EEG. The most important thing to know before getting a video EEG is that your healthcare team will always make sure you are safe during the testing. Other helpful tips include:
- Be sure you bathe or shower before starting the test. Once the electrodes are in place, you will not be able to wash your hair or shower.
- If you are going to the hospital, you may be there for several days, which can mean you’ll have quite a bit of down time. Make sure you bring items to keep you busy during your time at the hospital.
- Wear clothes that button or zip up so you don't have to pull them over your head. Remember, the EEG equipment is on your head!
- Ask the staff about use of electronic equipment. Usually a cell phone, laptop or other device can be used but not while it is plugged in. This is to avoid interfering with the EEG recordings and equipment.
- Ask the staff if someone should be with you. It helps to have a family member, friend, or caregiver stay with you during the testing. They can help observe seizures and point out characteristics to your healthcare team. This is done most often for children or for people with other disabilities that may not be able to stay alone in the hospital.
- Space out visits from family and friends. It's better to have people visit for a few hours at a time throughout the day rather than many people at once. This way they can keep you company and help observe seizures.
- Make sure you tell your healthcare team about all the medications you take and other health problems you may have. This information may affect how the EEG testing and medicine changes are done and what other care needs you may have.
- Having video EEG testing done in a hospital can be stressful. Make sure you tell the staff how you are feeling. Ask for help and ask questions! You may not get all the answers right away, but you'll have staff there to help you get through the testing in a safe and supportive way.
Video EEG Monitoring with Invasive Electrodes
What Happens If Scalp Electrodes Can’t Find Where Seizures Come From?
For some people, seizures can’t be found using scalp electrodes. The beginning of seizures may not be seen, or it’s possible that more than one area of the brain is involved. For example, EEG tests may show that seizures involve one of the frontal lobes of the brain. However, other tests suggest seizures in one of the temporal lobes. Another possibility is that seizure activity is seen on both sides of the brain. In these cases, we need to know if seizures are coming from both sides of the brain or if they start on one side but spread quickly to the other side. Surgery cannot be considered until more information is found.
When seizures can’t be easily found, "invasive electrodes" are placed under the skull and on the surface of the brain or into certain areas of the brain.
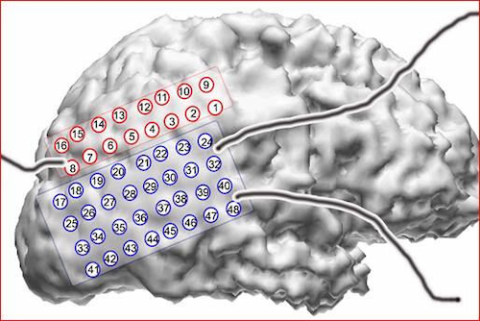
There are two main types of invasive electrodes: strips or grids and depth electrodes. These electrodes can pick up brain activity much better than scalp electrodes. They can also be used to map how the brain works near where the seizures start.
How Are Invasive Electrodes Placed?
Surgery is needed to place these invasive electrodes. Once the electrodes are placed, then the person is monitored via EEG. The surgery to place the electrodes may take only a few hours. Monitoring after placement may take a few days or a few weeks.
After the monitoring period, the electrodes are removed. Depending on the type of electrode used and results of testing, surgery may or may not be done. It’s not unusual for a person to be in the hospital for three weeks or so for this procedure and the EEG testing.
What Are Depth Electrodes And When Are They Used?
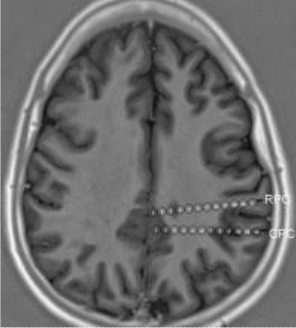
Depth electrodes are used if seizures start in deeper areas of the brain and not on the surface. Depth electrodes are thin wires that look like a needle. Each electrode can record from a number of sites along the electrode. The number of electrodes used will vary depending on what test results suggest for each person. For example, a person could have two to four electrodes placed on each side of the brain. They are placed in specific areas of the brain that are selected based on scalp EEG monitoring, MRI scans, and other tests.
To place depth electrodes, surgery is needed. A person can expect the following for depth electrode surgery:
- General anesthesia is given to put the person to sleep.
- A frame is then placed on the person’s head to help the surgeon find the exact place to put the electrodes.
- Very small holes are made in the skull and the electrodes are placed through these.
- Once in place, the electrodes are secured into the bone of the skull.
- A head dressing is placed over the electrodes and the wires that lead to the EEG monitoring equipment.
How Are Subdural Strips Or Grids Placed And When Are They Used?
If the seizure activity is thought to be on the surface of the brain, electrodes called strips or grids are used. They can record electrical activity from many points on the strip or grid. A strip may look like a rectangle, similar to the size of a small band aid. A grid is usually shaped like a square and can cover larger areas of the brain.
Surgery is a bit different to place the strips or grids. A person can expect the following for strip or grid surgery:
- General anesthesia is given to put the person to sleep.
- A larger opening in the skull is made (called a craniotomy) and the strips or grid are placed on the surface of the brain.
- Small thin wires attached to the strips or grids connect to the EEG equipment and are wrapped in the head dressing.
- The person then goes to the epilepsy monitoring unit to be recorded over a number of days.
What Else Are Invasive Electrodes Used For?
Brain mapping and electrical stimulation is a procedure that also uses strip, grid, and depth electrodes to map brain function. During this procedure, each point on the strip, grid, or depth electrode is stimulated with a brief, tiny electrical current. The person is watched for changes in movement, strength, language, and vision. A map is made based on the location of each stimulation point. This helps understand the function of those brain areas and if surgery is safe to do. Once enough information is recorded, the electrodes are removed and a decision about surgery can be made.
What Are the Risks of Having Invasive Electrodes Placed?
Depth electrodes have a very small risk of complications. Smaller holes are made in the skull so people may recover quicker and have less pain or discomfort than after grids or strips. Possible, yet infrequent, complications may include bleeding in the brain and infection. The potential for complications and headaches after surgery is slightly greater since surgery to place strips or grids needs a larger opening in the brain.
Resources
Epilepsy Centers
Epilepsy centers provide you with a team of specialists to help you diagnose your epilepsy and explore treatment options.
Epilepsy Medication
Find in-depth information on anti-seizure medications so you know what to ask your doctor.
Epilepsy and Seizures 24/7 Helpline
Call our Epilepsy and Seizures 24/7 Helpline and talk with an epilepsy information specialist or submit a question online.
Tools & Resources
Get information, tips, and more to help you manage your epilepsy.



