Hypothalamic Hamartoma
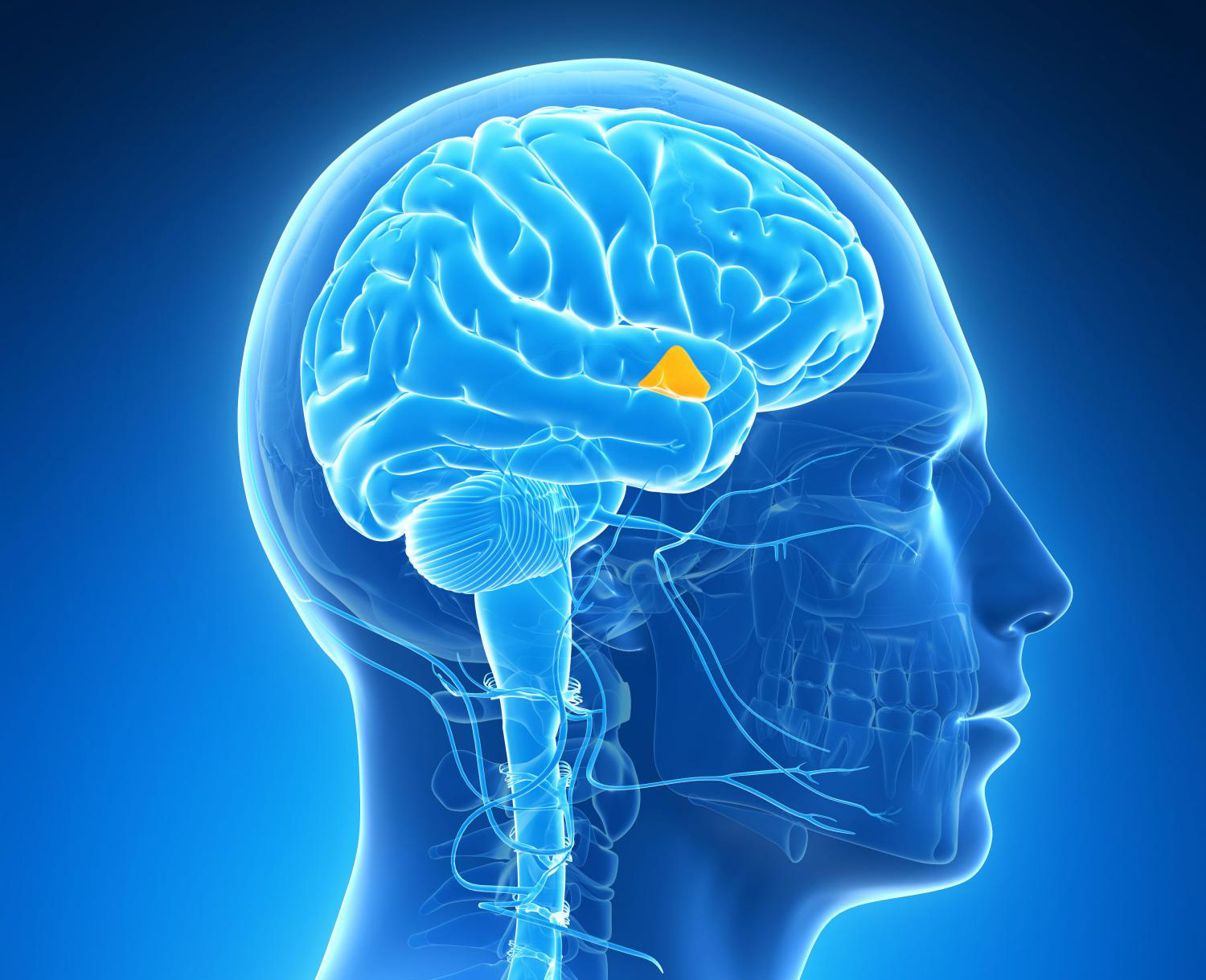
Located at the base of the brain, the hypothalamus regulates many of the “automatic” functions of the brain, including hunger, thirst, temperature, passion, and hormone regulation. It’s also involved in hormone balance.
What Is A Hypothalamic Hamartoma?
A hypothalamic hamartoma (HH) is a rare, benign (noncancerous) brain tumor or lesion of the hypothalamus. The hypothalamus is located at the base of the brain and regulates many of the “automatic” functions of the brain, including hunger, thirst, temperature, passion, and hormone regulation. It’s also involved in hormone balance.
A hypothalamic hamartoma can cause many types of seizures and other symptoms. The symptoms can vary from one person to the next. Many people have some combination of the following problems:
- Gelastic or dacrystic seizures (focal seizures with laughing or crying)
- Other seizure types, such as absence, atonic, tonic, or tonic-clonic
- Cognitive problems, such as changes in thinking, memory, attention)
- Sudden episodes of rage (called hypothamaic rages)
- Other types of changes in mood or behavior
- Precocious or early puberty
- Pallister-Hall syndrome (a genetic condition that may include a number of problems, such as extra fingers or toes, changes in pituitary or hormone function, and changes in the way the head, face, and other parts of the body develop)
How Often Does HH Occur?
- While the exact number of people with hypothalamic hamartomas is not known, HH is estimated to occur in 1 out of 200,000 children and teenagers worldwide.
- This estimate, which may be low since HH is hard to detect, suggests that there are about 30,000 in the world living with HH.
What Causes HH?
We don’t yet know the cause of HH. Hamartomas are considered benign, which means they don’t usually get larger. Seizures and other health problems can affect a person’s health and life in many ways.
Some research suggests that certain mutations or changes in the GL13 gene may be involved.
- Mutations can be germline (changes in genes found in all cells) or somatic (changes seen only in some groups of cells).
- Some gene research suggests that some cases of HH may be linked with somatic mutations of the GLI3 gene in the tissue of the hamartoma.
How Is HH Diagnosed?
Hypothalamic hamartomas can be hard to diagnose and even more difficult to treat.
- A misdiagnosis or delay in proper diagnosis may lead to wrong tests and procedures, worsening health and quality of life, and cognitive decline that can’t be reversed.
- The diagnosis of HH has improved with better ways to image or look at the brain.
How Is HH Treated?
Seizures in people with HH often don’t respond well to seizure medications, but newer surgical options have helped many people in the past decade. Treatment now focuses on:
- Reducing the size of the tumor in some people or removing it if possible.
- Controlling seizures, hopefully so the person has no more seizures or at least has significantly fewer.
- Stopping the decline or worsening of cognitive function.
It’s important to realize that treatments are not available or don’t work well for some people. When this happens, treatment is aimed at controlling and managing symptoms as best as possible with the least amount of side effects.
What Types Of Surgery Are Available?
Surgery with a craniotomy (making an opening in the skull to remove the hamartoma) has had poor outcomes in the past. Newer approaches with more promising results have been developed including:
- Transcallosal anterior inteforniceal surgery, developed in Australia by Dr. Jeffrey Rosenfeld
- Stereotactic thermoablation, favored by neurosurgeons in Japan
- Gamma knife radiosurgery
- MR-guided stereotactic laser thermoablation, a recent approach that is less invasive and seems to have better seizure free outcomes, shorter hospital stays, and fewer side effects
- Focused ultrasound, being tested in clinical trials
The type of surgery recommended for a person with HH is chosen based on a number of factors, such as the size and location of the hamartoma, seizure frequency, and cognitive function. A large hamartoma typically requires surgeries in different phases or a combined approach.
What Is The Outlook?
Some people with HH will have only a few seizures and minor cognitive and behavioral problems. However, most people will have seizures that are poorly controlled with medicines.
- People may show signs of more cognitive and behavior problems when seizure control is worse. These behavior problems may include unprovoked rage attacks, problems with social relationships, and difficulties in school or work.
- Infants and young children with HH may miss critical developmental milestones in speech, crawling, walking, and cognitive development.
What types of care and help are needed?
Managing the challenges often requires a team of knowledgeable medical specialists, including neurologists or epileptologists, neurosurgeons, neuropsychologists, endocrinologists, and pediatricians. These can be found at comprehensive epilepsy centers.
- The team of medical specialists will be crucial in managing the seizures - either through medications or surgery - as well as the endocrine or hormonal balance.
- Other specialists may be needed to help manage practical life skills issues, mood, behavioral concerns, and how HH can affect the individual’s and family quality of life.
- Specialists in HH are most likely found at pediatric epilepsy centers. These organizations can help you find an epilepsy specialist:
Resources
Epilepsy Centers
Epilepsy centers provide you with a team of specialists to help you diagnose your epilepsy and explore treatment options.
Epilepsy Medication
Find in-depth information on anti-seizure medications so you know what to ask your doctor.
Epilepsy and Seizures 24/7 Helpline
Call our Epilepsy and Seizures 24/7 Helpline and talk with an epilepsy information specialist or submit a question online.
Tools & Resources
Get information, tips, and more to help you manage your epilepsy.



